June
Is Crispr the Next Antibiotic?
By Knvul Sheikh
For decades, scientists and doctors have treated common bacterial and viral infections with fairly blunt therapies. If you developed a sinus infection or a stomach bug, you would likely be given a broad-spectrum antibiotic that would clear out many different types of bacteria. Antiviral drugs help treat viral illnesses in much the same way, by hindering the pathogen’s ability to reproduce and spread in the body.
But microorganisms are quick to evolve, and many have developed defenses against the methods devised to kill them. An increasing number of bacteria are now resistant to one or more antibiotics. Each year roughly 700,000 people around the world die from such infections, and by 2050 the number could rise to 10 million, according to United Nations estimates. Viruses, too, quickly evolve new ways of disguising themselves from drugs, often by hiding inside host cells. Less than 100 antiviral drugs have successfully made it all the way to the clinic since the first was approved in 1963.
Desperate to find new medicines against pathogenic microorganisms, scientists are turning to Crispr, the gene-editing tool. Crispr has typically been considered for macroscopic tasks: altering mosquitoes so they can’t spread malaria, editing tomatoes so they are more flavorful and curing certain genetic diseases in humans. Now researchers are harnessing Crispr to turn a bacterium’s machinery against itself, or against viruses that infect human cells. “Crispr is the next step in antimicrobial therapy,” said David Edgell, a biologist at the Western University in London, Ontario, and the lead author of a study published earlier this month in Nature Communications.
Crispr is a specialized region of DNA that creates what amount to genetic scissors — enzymes that allow the cell (or a scientist) to precisely edit other DNA or its sister molecule, RNA. (Crispr is shorthand for “clustered regularly interspaced short palindromic repeats.”) Crispr was originally discovered in bacteria, where it helps keep track of past injury. When a virus attacks, the bacterium stores small chunks of the viral genome within its own DNA. This helps the bacterium recognize viral infections when they occur again. Then, using Crispr-associated enzymes, it can disarm the virus and prevent the infection from spreading.
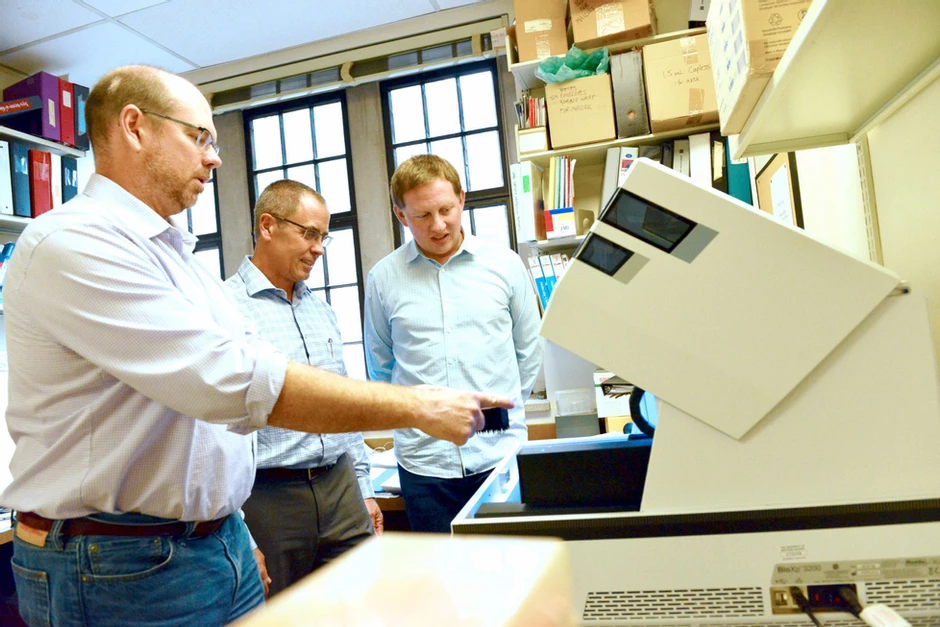
In their recent study, Dr. Edgell and his colleagues successfully used a Crispr-associated enzyme called Cas9 to eliminate a species of Salmonella. By programming the Cas9 to view the bacterium itself as the enemy, Dr. Edgell and his colleagues were able to force Salmonella to make lethal cuts to its own genome.
The team began with a conjugated plasmid — a small packet of genetic material that can replicate itself and be passed from one bacterium to the next. To the plasmid the scientists added the encoded instructions for Crispr enzymes that would target Salmonella DNA. The plasmid was then tucked inside E. coli bacteria. Dr. Edgell reasoned that most types of E. coli are typically part of a healthy gut microbiome, and would already be present if a person ingested pathogenic Salmonella by, say, eating a contaminated salad. The E. coli could then transfer the engineered plasmid to the Salmonella, where the Crispr system would activate, destroying the bad bacteria.
That is exactly what the researchers observed in a petri dish. The Crispr system wiped out nearly all Salmonella bacteria, while leaving E. coli intact. “This represents a significant advance in being able to target bacteria in a highly specific way,” said Mitch McVey, a biologist at Tufts University who was not involved in the study.
Crispr-based antibiotic pills aren’t yet anywhere near pharmacy shelves. But developing such treatments could allow scientists to harness the power of the human body’s own resident microbes in preventing disease. “Scientists are starting to figure out that microbiota can also be extremely beneficial for our health,” said Luciano Marraffini, a microbiologist at Rockefeller University and the Howard Hughes Medical Institute.
Conventional antibiotics do not distinguish between good and bad bacteria, eradicating everything indiscriminately and occasionally creating problems for people with weakened immune systems. “A major benefit of Crispr is that we can program it to kill only specific pathogenic bacteria and leave alone the rest of our healthy microbes,” Dr. Marraffini said.
A few companies have started to pursue Crispr-based antibiotics that can be delivered through viruses that have been engineered so that they cannot reproduce or cause infections themselves, as well as other methods. Dr. Marraffini is a co-founder of one such start-up, Eligo Bioscience. The specificity of Crispr is equally enticing to researchers looking to target pathogenic viruses. Instead of having Crispr kill viruses that infect bacteria, as it does in nature, scientists are programming it to chop up viruses that infect humans. In a study, also published this month in Molecular Cell, scientists at the Broad Institute of M.I.T. and Harvard demonstrated that another Crispr enzyme, Cas13, could be programmed to detect and kill three different single-stranded RNA viruses that infect human cells: influenza A virus, lymphocytic choriomeningitis virus and vesicular stomatitis virus.
Using this Crispr system, researchers saw up to a 40-fold reduction in viral RNA within 24 hours. The enzymes damaged the viral genomes significantly enough that few viruses could infect new cells. In the case of the flu virus, Cas13 reduced its infectiousness by more than 300-fold. “This is a great proof-of-concept,” said Rodolphe Barrangou, a microbiologist at North Carolina State University, who also co-founded a company for Crispr-based antimicrobial products and was not involved in the study. If researchers can design Crispr technology against three fairly mild human viruses, such as influenza, lymphocytic choriomeningitis virus and vesicular stomatitis virus, they can likely modify it to treat more deadly viral infections as well.
Compared to current antiviral drugs, Crispr has the advantage of being easy to tweak as needed. “If a virus evolves and mutates, we can simply change the Crispr system to match whatever the virus is doing,” said Cameron Myhrvold, a postdoctoral researcher at Broad. Now researchers face the challenge of demonstrating that Crispr antibacterial and antiviral drugs are effective in living animals and in humans, not just in the lab, and that they will be cheaper than conventional therapies, Dr. Barrangou said. “We’re not ready for clinical prime time yet,” he said. “But we’re getting there.”
More Details: https://mediarelations.uwo.ca/2019/10/04/researchers-unlock-potential-to-use-crispr-to-alter-the-human-microbiome/



Leave a Reply